Verwandte Artikel zu Called for Life: How a Loving Neighbour Led Us Into...
Zu dieser ISBN ist aktuell kein Angebot verfügbar.
Alle Exemplare der Ausgabe mit dieser ISBN anzeigen:him that, he smiled and said, It wasn t that great for me either! But Kent gives
God the credit for saving his life and surviving the deadly Ebola virus that infected
him while serving others in the name of Jesus. Dr. Brantly and his wife, Amber,
went obediently to Liberia to serve with Samaritan s Purse as medical missionaries,
and were the recipients of prayers from around the world as they battled an attack
that threatened their future. The world watched as Kent was successfully trans ported back to the United States from Africa. International media outlets captured
his every step as he walked from the ambulance into Atlanta s Emory University
Hospital, where he found physical restoration a miracle from God. You will be
riveted by this extraordinary couple who are called for life to serve the Lord Jesus
Christ the Great Physician! Franklin Graham, president and CEO, Samaritan s Purse
and Billy Graham Evangelistic Association
When hope seems dim, Called for Life reminds us of the limitless possibilities of
a God- driven life. Dr. Brantly s story inspires us to stay strong in the unexpected
crises of life, to be encouraged to recall God s promises, to be challenged to
examine our own commitment to God s call on our lives. Max Lucado, pastor and best-selling author
Compelling, factual, and emotional, Called for Life draws readers to reflect on their own journeys to faith in Christ and encourages them to trust God in the
crises of life. Nancy Writebol, SIM missionary to Liberia and fellow Ebola survivor
Kent and his wife, Amber, have truly lived by the phrase When the going gets
tough, the tough go back to their calling. Their great compassion for the sick and
broken choosing to suffer alongside them even in the face of possible death
has touched and saved many lives. I am thrilled to see the Brantlys share their amazing story in print, and I know it will inspire and challenge you to find your place in God s calling upon your life. Dr. Ravi Zacharias, author and speaker
"Called for Life invites all of us behind the curtain of the news stories and press
releases and into the Brantlys lives during the most trying of times. Their love
for each other, their faith and courage, as well as the strength and support they received from their network of friends, family, and caregivers is heartwarming and inspiring. When we set out to just do what is right, this behind-the-news-flash story reminds all of us that we live in a global community, that we all have a role to play, and that all of us can make a difference, wherever we are and in whatever profession."
Lisa Hensley, virologist and deputy director at the National Institute of Allergy and Infectious Disease, Integrated Research Facility
As you walk alongside them on their journey, Kent and Amber s poignant story
will touch your heart, move you to tears, strengthen your faith, and cause you to
trust God more. David Stevens, MD, MA (Ethics), CEO of the Christian Medical and Dental Associations
"Called for Life tells the rest of the story what went before, lay behind, and follows after the iconic images of a coverall clad figure gently stepping out of an ambulance and into an international spotlight. Kent and Amber have given us a glimpse inside their previously private world to uncover the roots of their genuine humility, tender love for each other, and deep compassion for their neighbors. Not all readers will fully resonate with their interpretations, but all will surely appreciate their candor, sensitivity, and sincerity, and the beauty, and suspense of a story well told. David McRay, MD, professor at the University of Tennessee College of Medicine
There are many books about surviving illness, but this is a one-of-a-kind story.
What happens when ordinary Christian medical missionaries are caught up in an
extraordinary world crisis? Though I know the story, I found my heart pounding
as I turned the pages. And it turns out to be a tale not of disease, primarily, but of
calling, faith, and love. It is a story of a remarkable family, their community, and
their commitment to a hurting world and to God. Randy Harris, spiritual director and instructor, Abilene Christian University
Knowing Kent and Amber personally, I can say that Called for Life is a deep and
honest testament to God s working in the midst of suffering and crisis. Kent and
Amber s voices come through the pages in a very authentic way, and you will experience all Kent s emotions as he walks through this journey. As an Ebola survivor myself, I wholeheartedly recommend this book. Rick Sacra, MD, SIM missionary
Refreshingly, the Brantlys never give trite answers to complex questions like How
does God work in healing? or Why is there suffering in the world? Instead, what they give us is a story their story, and it s one worth reading. Jonathan Storment, preaching minister at the Highland Church of Christ and co-author of Bringing Heaven to Earth"
—Dr. Kent Brantly, in Called for Life
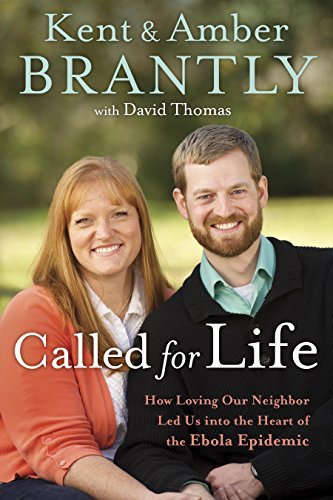
Just months after Dr. Kent Brantly arrived in Liberia with his wife, Amber, and their two children, the Ebola virus erupted in West Africa. Kent and his colleagues began to fight one of the most horrifying, incurable diseases on earth, only to see patient after patient die. Then, after six weeks of intense battle to help others survive, Kent woke up one July morning with a fever. Three days later his diagnosis was confirmed: Ebola.
Kent knew his life was at stake. He also knew Amber, family members, and friends were praying desperately. What he didn’t know was that his case would make international headlines as he was evacuated to Atlanta, becoming the first person with Ebola ever treated in the United States. He didn’t know he would be the center of a media firestorm of debate, questions, and fears. And he didn’t know that his faith would inspire people around the world to trust in a faithful God.
“Kent, bud. We got your test result. And I’m really sorry to tell you that it is positive for Ebola.”
--From the Prologue, Called for Life
Dr. Kent and Amber Brantly moved with their children to war-torn Liberia in the fall of 2013 to provide medical care for people in great need—to help replace hopelessness with hope. When, less than a year later, Kent contracted the deadly Ebola virus, hope became what he and Amber needed too.
When Kent received the diagnosis, he was already alone and in quarantine in the Brantly home in Liberia. Amber and the children had left just days earlier on a trip to the United States. Kent’s personal battle against the horrific Ebola began, and as thousands of people worldwide prayed for his life, a miraculous series of events unfolded.
Called for Life tells the riveting inside story of Kent and Amber’s call to serve their neighbors, as well as Kent’s fight for life with Ebola and Amber’s’ struggle to support him from half-a-world away. Most significantly,Called for Life reminds us of the risk, the honor, and the joy to be known when God and others are served without reservation.
„Über diesen Titel“ kann sich auf eine andere Ausgabe dieses Titels beziehen.
- VerlagWaterbrook Press (A Division of Random House Inc)
- Erscheinungsdatum2015
- ISBN 10 1601428235
- ISBN 13 9781601428233
- EinbandTapa dura
- Auflage1
- Anzahl der Seiten240
- Bewertung
Versand:
EUR 5,61
Von Vereinigtes Königreich nach USA
Beste Suchergebnisse beim ZVAB
Called for Life: How a Loving Neighbour Led Us Into the Heart of the Ebola Epidemic
Buchbeschreibung Paperback. Zustand: Very Good. The book has been read, but is in excellent condition. Pages are intact and not marred by notes or highlighting. The spine remains undamaged. Artikel-Nr. GOR008905446
Weitere Informationen zu diesem Verkäufer | Verkäufer kontaktieren
Called for Life: How a Loving Neighbour Led Us Into the Heart of the Ebola Epidemic
Buchbeschreibung Paperback. Zustand: Good. The book has been read but remains in clean condition. All pages are intact and the cover is intact. Some minor wear to the spine. Artikel-Nr. GOR010494179
Weitere Informationen zu diesem Verkäufer | Verkäufer kontaktieren
Called for Life : How Loving Our Neighbor Led Us into the Heart of the Ebola Epidemic
Buchbeschreibung Zustand: Very Good. 1st Edition. Former library book; may include library markings. Used book that is in excellent condition. May show signs of wear or have minor defects. Artikel-Nr. 10510517-75
Weitere Informationen zu diesem Verkäufer | Verkäufer kontaktieren
Called for Life : How Loving Our Neighbor Led Us into the Heart of the Ebola Epidemic
Buchbeschreibung Zustand: Good. 1st Edition. Used book that is in clean, average condition without any missing pages. Artikel-Nr. 5602835-75
Weitere Informationen zu diesem Verkäufer | Verkäufer kontaktieren
Called for Life: How a Loving Neighbour Led Us Into the Heart of the Ebola Epidemic
Buchbeschreibung Zustand: VeryGood. Most items will be dispatched the same or the next working day. Artikel-Nr. wbs8186928302
Weitere Informationen zu diesem Verkäufer | Verkäufer kontaktieren
Called for Life: How Loving Our Neighbor Led Us Into the Heart of the Ebola Epidemic
Buchbeschreibung Befriedigend/Good: Durchschnittlich erhaltenes Buch bzw. Schutzumschlag mit Gebrauchsspuren, aber vollständigen Seiten. / Describes the average WORN book or dust jacket that has all the pages present. Artikel-Nr. M01601428235-G
Weitere Informationen zu diesem Verkäufer | Verkäufer kontaktieren

